
Early Signs of Arthritis in Feet
 Arthritis causes inflammation and stiffness in the joints. There are many different types of arthritis, but the types of arthritis that most often affect the feet are osteoarthritis, rheumatoid arthritis, psoriatic arthritis, and gout. Arthritis progressively worsens over time, but the earlier it is detected, the sooner measures can be taken to slow its progression and preserve the health of your feet. The earliest signs of arthritis are joint stiffness, pain, swelling, and warmth. Sometimes the joints may begin to appear deformed or develop bone spurs. If you suspect that you may have arthritis in your feet, please consult with a podiatrist, who can help you manage this condition.
Arthritis causes inflammation and stiffness in the joints. There are many different types of arthritis, but the types of arthritis that most often affect the feet are osteoarthritis, rheumatoid arthritis, psoriatic arthritis, and gout. Arthritis progressively worsens over time, but the earlier it is detected, the sooner measures can be taken to slow its progression and preserve the health of your feet. The earliest signs of arthritis are joint stiffness, pain, swelling, and warmth. Sometimes the joints may begin to appear deformed or develop bone spurs. If you suspect that you may have arthritis in your feet, please consult with a podiatrist, who can help you manage this condition.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact John Killough, DPM from Regional Foot Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a joint disorder that involves the inflammation of different joints in your body, such as those in your feet. Arthritis is often caused by a degenerative joint disease and causes mild to severe pain in all affected areas. In addition to this, swelling and stiffness in the affected joints can also be a common symptom of arthritis.
In many cases, wearing ill-fitting shoes can worsen the effects and pain of arthritis. Wearing shoes that have a lower heel and extra room can help your feet feel more comfortable. In cases of rheumatoid arthritis, the arch in your foot may become problematic. Buying shoes with proper arch support that contour to your feet can help immensely.
Alleviating Arthritic Pain
- Exercises that stretch the foot can prevent further pain and injury and increase mobility
- Most of the pain can be alleviated with anti-inflammatory drugs, heat, and topical medications
- Massages can help temporarily alleviate pain.
It is best to see your doctor for the treatment that is right for your needs and symptoms. Conditions vary, and a podiatrist can help you determine the right method of care for your feet.
If you have any questions, please feel free to contact our offices located in Charleston and Effingham, IL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Arthritic Foot Care
During your lifetime, you will probably walk about 75,000 miles, which is quite a lot of stress to put on your feet. As you get older, the 26 bones and 30 joints in each of your feet will lose flexibility and elasticity. Your foot’s natural shock absorbers will wear down as well. Having arthritis added to this mix only makes matters worse. Your joints will become distorted and inflamed, which is why arthritic foot care needs to be something to think about every day.
When dealing with arthritis, having additional foot complications, such as bunions, hammertoes, or neuroma, can be a serious detriment. To avoid these, buy well-fitting shoes with a lower heel and good support. Arthritis causes you to lose your arch, so having shoes with good arch support is also highly recommended.
Aside from getting good arch support, the shoes need to fit comfortably and properly as well. A good place to start is by leaving a finger width between the back of the shoe and your foot to gauge proper size. It is also helpful to have a square or rounded toe box in the front to provide even more comfort. Another thing to look for is a rubber sole that can provide a cushion and absorb shock as you walk. This adds flexibility to the ball of your foot when you push off your heel to walk.
Exercise is another key aspect of arthritic foot care. Exercise not only strengthens and stretches your muscles and joints, but helps to prevent further injury and pain as well. Stretching the Achilles tendon, the tendon located in the back of your heel, will give you added mobility and reduce pain due to stress. Another thing you can do is massage your feet, kneading the ball of your foot as well as your toes from top to bottom.
Stretching the Achilles tendon is a simple exercise that you can do at home anytime. Lean against the wall with your palms flat against the surface while placing one foot forward, towards the wall, and one foot behind you. Bend your forward knee towards the wall while keeping your back knee locked straight, and make sure both your heels are completely touching the ground at all times. This will stretch your Achilles tendon and calf muscles as well. You will feel the stretch almost immediately. You can also stretch your toes in a couple ways. One involves taking a rubber band and wrapping it around both your big toes while your heels remain together. Then, pull them apart to stretch your big toe. You can also place a rubber band around all the toes of one of your feet. Then, try to separate each individual toe, stretching them all.
A final step you can take to help your arthritis is taking non-steroid, non-inflammatory drugs or topical medicines with capsaicin. Unfortunately, there is no complete way to remove all of your arthritic pain. However, following some of this advice can go a long way in staying as pain-free as possible.
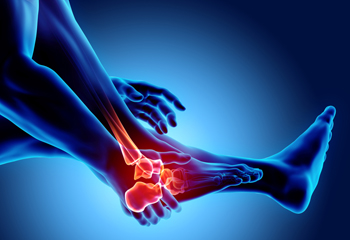
Types of Ankle Sprains
Ankle sprains occur when the ligaments in the ankle tear. They are particularly common among athletes and can cause pain and swelling in the affected leg that make moving the ankle and bearing weight very difficult. There are two types of ankle sprains. In an eversion ankle sprain, the ankle rolls outward and tears the deltoid ligaments. In an inversion sprain, the ankle rolls inward while the foot is twisted upwards. Inversion ankle sprains are more common than eversion ankle sprains. Ankle sprains are also classified by where in the ankle they occur, and the extent of the damage. If you suspect that you have sprained your ankle it is recommended that you see a podiatrist for a proper diagnosis and treatment.
Although ankle sprains are common, they aren’t always minor injuries. If you need your ankle injury looked at, contact John Killough, DPM from Regional Foot Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains are the result of a tear in the ligaments within the ankle. These injuries may happen when you make a rapid shifting movement while your foot is planted. A less common way to sprain your ankle is when your ankle rolls inward while your foot turns outward.
What Are the Symptoms?
- Pain at the sight of the tear
- Bruising/Swelling
- Ankle area is tender to touch
- In severe cases, may hear/feel something tear
- Skin discoloration
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
In many cases, the RICE method (Rest, Ice, Compression, and Elevate) is used to treat ankle sprains. However, you should see a podiatrist to see which treatment option would work best with your injury. In severe cases, surgery may be required.
It is important to ask your doctor about rehab options after you receive treatment for your injury. Stretching, strength training, and balance exercises may help the ankle heal while also preventing further injury.
If you have any questions, please feel free to contact our offices located in Charleston and Effingham, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Sprains
Although ankle sprains may not be as serious as a broken ankle, they should be given immediate attention and care. An ankle sprain can lead to a significant amount of pain, as well as limited mobility. They are often characterized by the swelling and discoloration of the skin. This occurs when the ligaments are stretched beyond their limits.
The simple act of walking can sometimes cause a sprain, which makes ankle sprains a very common injury that can happen to anyone. They occur when the ankle twists in an awkward way or rolls over itself, causing a pop or snap in the tendons around the ankle. Some people are more at risk than others. These include athletes who continually push their bodies to the limits and also people who have previously suffered accidents to the feet, ankles, or lower legs.
Most of the time, an ankle sprain is not severe enough for hospital attention. There are many at-home treatment options available, including propping the leg up above your head to reduce blood flow and inflammation, applying ice packs to the affected area as needed, taking over-the-counter pain relievers and anti-inflammatory medication, using an ACE bandage to wrap and support the injured ankle, and most importantly, remaining off your feet until the ankle has fully healed.
Despite this, an ankle sprain can turn into a severe injury that might require hospitalization. If the ankle ligaments or muscles are damaged from a tear or rip, that is one sign that the sprain is severe enough for hospital attention and possibly for surgery. Even after the surgery, the recovery process can be long. You may need to have rehabilitation sessions administered by your podiatrist to get your ankle back to full health.
The severity of your sprain might become apparent if you are unable to stand or walk, consistent pain occurs over a prolonged period of time, swelling is much more severe than initially present, or if you start to experience tingling or numbness. These signs may indicate that your ankle sprain might actually be a broken ankle, an injury that requires immediate medical attention.
Although they are not completely avoidable, ankle sprains can be curbed with some preventative treatment measures. These include wearing appropriate-fitting shoes that not only provide a comfortable fit, but also ankle support. It is also recommended to stretch before doing any kind of physical activity, as this will help lower your body’s chance for an injury.
Who Does Sever’s Disease Affect?
 An injury to the growth plate in the heel may indicate a condition that is known as Sever’s disease. It generally affects children and young teenagers who participate in sporting activities. The heel can become inflamed, which can cause severe pain and discomfort. Mild relief may be found when the activity that caused the injury is temporarily stopped, and walking patterns may be changed. It may help to wear custom made orthotics if Sever’s disease is severe, and some patients find it necessary to take pain medication. If your child complains of heel pain, please consult with a podiatrist who can properly diagnose and treat Sever's disease.
An injury to the growth plate in the heel may indicate a condition that is known as Sever’s disease. It generally affects children and young teenagers who participate in sporting activities. The heel can become inflamed, which can cause severe pain and discomfort. Mild relief may be found when the activity that caused the injury is temporarily stopped, and walking patterns may be changed. It may help to wear custom made orthotics if Sever’s disease is severe, and some patients find it necessary to take pain medication. If your child complains of heel pain, please consult with a podiatrist who can properly diagnose and treat Sever's disease.
Sever's disease often occurs in children and teens. If your child is experiencing foot or ankle pain, see John Killough, DPM from Regional Foot Center. Our doctor can treat your child’s foot and ankle needs.
Sever’s Disease
Sever’s disease is also known as calcaneal apophysitis, which is a medical condition that causes heel pain I none or both feet. The disease is known to affect children between the ages of 8 and 14.
Sever’s disease occurs when part of the child’s heel known as the growth plate (calcaneal epiphysis) is attached to the Achilles tendon. This area can suffer injury when the muscles and tendons of the growing foot do not keep pace with bone growth. Therefore, the constant pain which one experiences at the back of the heel will make the child unable to put any weight on the heel. The child is then forced to walk on their toes.
Symptoms
Acute pain – Pain associated with Sever’s disease is usually felt in the heel when the child engages in physical activity such as walking, jumping and or running.
Highly active – Children who are very active are among the most susceptible in experiencing Sever’s disease, because of the stress and tension placed on their feet.
If you have any questions, please feel free to contact our offices located in Charleston and Effingham, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle injuries.
Sever's Disease
Sever's disease, also known as calcaneal apophysitis, is a medical condition that causes heel pain in children’s feet while they’re growing. Sever's disease occurs most commonly in boys and girls between the ages of 8 and 14.
Sever's disease occurs when the child’s growth plate, or the calcaneal epiphysis, an area attached to the Achilles tendon, is injured or when the muscles and tendons of the growing foot do not keep pace with bone growth. The result is constant pain experienced at the back of the heel and the inability to put any weight on the heel. This forces the child to bear weight on their toes while walking. When a toe gait develops, the child must change the way they walk to avoid placing weight on the painful heel. If this is not properly addressed, this can lead to further developmental problems.
The most common symptom of Sever's disease is acute pain felt in the heel when a child engages in physical activity such as walking, jumping or running. Children who are active athletes are among the group most susceptible to experiencing Sever's disease. This is due to the extreme stress and tension placed on their growing feet. The rolling movement of the foot during walking or running and obesity are both additional conditions linked to causing Sever's disease.
The first step in treating Sever's disease is to rest the foot and leg and avoid physical activity. Over the counter pain-relieving and anti-inflammatory medications can be helpful for reducing the amount of heel pain. A child with Sever's disease should also wear shoes that properly support the heel and the arch of the foot. Consider purchasing orthotic shoe inserts which can help support the heel and foot while it is healing. Most patients with Sever's disease symptoms report an eventual elimination of heel pain after wearing orthotic insoles that support the affected heel.
Sever's disease may affect either one heel or both. It is important for a child experiencing heel pain to be examined by a foot doctor who can apply the squeeze test. The squeeze test compresses both sides of the heel in order to determine if there is intense pain. Discourage any child diagnosed with Sever's disease from going barefoot as this can intensify the problem. Apply ice packs to the affected painful heel two or three times a day for pain relief.
Exercises that help stretch the calf muscles and hamstrings are effective at treating Sever's disease. An exercise known as foot curling has also proven to be very effective at treating Sever's disease. When foot curling, the foot is pointed away from the body, then curled toward the body to help stretch the muscles. The curling exercise should be done in sets of 10 or 20 repetitions and repeated several times throughout the day.
Treatment methods can continue for at least 2 weeks and as long as 2 months before the heel pain completely disappears. A child can continue doing daily stretching exercises for the legs and feet to prevent Sever’s disease from returning.
How Does Morton’s Neuroma Affect the Feet?
 Many people have general aches and pains in their feet. When pain develops in the ball of the foot, it may be indicative of a condition that is referred to as Morton’s neuroma. This is an ailment that affects the nerves in the feet that helps to avoid falling by maintaining balance. It develops as a result of inflamed nerves which can happen for a variety of reasons. These can include wearing shoes that do not fit correctly or from medical ailments consisting of bunions, hammertoe, and flat feet. Mild relief may be found when the affected foot is massaged, and it may be beneficial to wear custom made orthotics. If you have pain in this part of your foot, it is strongly suggested that you seek the counsel of a podiatrist who can properly diagnose and treat Morton’s neuroma.
Many people have general aches and pains in their feet. When pain develops in the ball of the foot, it may be indicative of a condition that is referred to as Morton’s neuroma. This is an ailment that affects the nerves in the feet that helps to avoid falling by maintaining balance. It develops as a result of inflamed nerves which can happen for a variety of reasons. These can include wearing shoes that do not fit correctly or from medical ailments consisting of bunions, hammertoe, and flat feet. Mild relief may be found when the affected foot is massaged, and it may be beneficial to wear custom made orthotics. If you have pain in this part of your foot, it is strongly suggested that you seek the counsel of a podiatrist who can properly diagnose and treat Morton’s neuroma.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact John Killough, DPM of Regional Foot Center. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Charleston and Effingham, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Signs of Serious Foot Problems in Diabetics
 Serious foot problems can be more likely among people who have diabetes, and they can result in serious complications if left untreated. If you have diabetes, certain foot symptoms can be a cause for concern and should be examined by a professional. Tingling, burning, or numbness in the feet, a burning pain, a dull ache, a loss of sensation, foot swelling, and cramps in your calves when resting or walking are all signs of potentially serious problems. Symptoms that affect the skin of the lower limbs, such as having shiny, smooth skin on the feet, hair loss, a lack of sweat, or wounds and sores on the feet that don’t heal are also a cause for concern. Additionally, if you see changes in the color, shape, or temperature of your feet, notice a cut or blister that you can see but can’t feel, or smell a foul odor coming from a wound, then you should seek immediate medical attention. A podiatrist can help you take care of your feet.
Serious foot problems can be more likely among people who have diabetes, and they can result in serious complications if left untreated. If you have diabetes, certain foot symptoms can be a cause for concern and should be examined by a professional. Tingling, burning, or numbness in the feet, a burning pain, a dull ache, a loss of sensation, foot swelling, and cramps in your calves when resting or walking are all signs of potentially serious problems. Symptoms that affect the skin of the lower limbs, such as having shiny, smooth skin on the feet, hair loss, a lack of sweat, or wounds and sores on the feet that don’t heal are also a cause for concern. Additionally, if you see changes in the color, shape, or temperature of your feet, notice a cut or blister that you can see but can’t feel, or smell a foul odor coming from a wound, then you should seek immediate medical attention. A podiatrist can help you take care of your feet.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact John Killough, DPM from Regional Foot Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Charleston and Effingham, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Care
Diabetes can cause two problems that can potentially affect the feet: Diabetic neuropathy and Peripheral Vascular Disease. Diabetic neuropathy occurs when nerves in your legs and feet become damaged, which prevents you from feeling heat, cold, or pain. The problem with diabetic neuropathy is that a cut or sore on the foot may go unnoticed and the cut may eventually become infected. This condition is also a main cause of foot ulcers. Additionally, Peripheral vascular disease also affects blood flow in the body. Poor blood flow will cause sores and cuts to take longer to heal. Infections that don’t heal do to poor blood flow can potentially cause ulcers or gangrene.
There are certain foot problems that are more commonly found in people with diabetes such as Athlete’s foot, calluses, corns, blisters, bunions, foot ulcers, ingrown toenails, and plantar warts. These conditions can lead to infection and serious complications such as amputation. Fortunately, proper foot care can help prevent these foot problems before they progress into more serious complications.
Each day you should wash your feet in warm water with a mild soap. When you finish washing your feet, dry them carefully especially between your toes. You should also perform daily foot inspections to ensure you don’t have any redness, blisters, or calluses. Furthermore, if you are diabetic, you should always wear closed-toed shoes or slippers to protect your feet. Practicing these tips will help ensure that your feet are kept healthy and away from infection.
If you have diabetes, contact your podiatrist if you have any of the following symptoms on your feet: changes in skin color, corns or calluses, open sores that are slow to heal, unusual and persistent odor, or changes in skin temperature. Your podiatrist will do a thorough examination of your feet to help treat these problematic conditions.
Understanding Orthotics
 Orthotics are shoe inserts that are designed to relieve pain that is caused by a foot condition. Orthotics can help to treat a variety of ailments, such as corns and calluses, tendonitis, bunions, heel pain, and recurring stress fractures. Orthotics may also be used to help correct posture and alignment issues as needed. Types of orthotics can include prefabricated or custom orthotics, cushioned orthotics to provide shock absorption, and pressure relief orthotics that redistribute body weight across the sole of the foot. When prescribing orthotics, a podiatrist will consider a variety of factors, including existing foot conditions, foot structure, biomechanics, the type of shoes normally worn, and lifestyle factors. If you believe that orthotics may be helpful for your foot-related issues, don’t hesitate to visit a podiatrist for more information.
Orthotics are shoe inserts that are designed to relieve pain that is caused by a foot condition. Orthotics can help to treat a variety of ailments, such as corns and calluses, tendonitis, bunions, heel pain, and recurring stress fractures. Orthotics may also be used to help correct posture and alignment issues as needed. Types of orthotics can include prefabricated or custom orthotics, cushioned orthotics to provide shock absorption, and pressure relief orthotics that redistribute body weight across the sole of the foot. When prescribing orthotics, a podiatrist will consider a variety of factors, including existing foot conditions, foot structure, biomechanics, the type of shoes normally worn, and lifestyle factors. If you believe that orthotics may be helpful for your foot-related issues, don’t hesitate to visit a podiatrist for more information.
If you are having discomfort in your feet and would like to try orthotics, contact John Killough, DPM from Regional Foot Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our offices located in Charleston and Effingham, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.











