Preventing Falls
 Falls are common incidents that can lead to serious injuries, especially in older adults. They occur due to various factors, including poor balance, muscle weakness, vision problems, medication side effects, and environmental hazards like slippery floors or loose rugs. The elderly, particularly those with chronic conditions such as arthritis, osteoporosis, or diabetes, are most at risk. As a result of falls, the feet can suffer fractures, sprains, and bruises, which can significantly impair mobility and independence. Preventing falls involves regular exercise to improve strength and balance, ensuring homes are free of tripping hazards, and wearing supportive footwear. Vision checks and reviewing medications with healthcare providers can also help reduce risks. If a fall occurs, immediate treatment includes rest, compression, and elevation for minor injuries. If you have injured your feet from a fall, it is suggested that you visit a podiatrist for treatment and additional fall prevention tips.
Falls are common incidents that can lead to serious injuries, especially in older adults. They occur due to various factors, including poor balance, muscle weakness, vision problems, medication side effects, and environmental hazards like slippery floors or loose rugs. The elderly, particularly those with chronic conditions such as arthritis, osteoporosis, or diabetes, are most at risk. As a result of falls, the feet can suffer fractures, sprains, and bruises, which can significantly impair mobility and independence. Preventing falls involves regular exercise to improve strength and balance, ensuring homes are free of tripping hazards, and wearing supportive footwear. Vision checks and reviewing medications with healthcare providers can also help reduce risks. If a fall occurs, immediate treatment includes rest, compression, and elevation for minor injuries. If you have injured your feet from a fall, it is suggested that you visit a podiatrist for treatment and additional fall prevention tips.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with John Killough, DPM from Regional Foot Center. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our offices located in Charleston and Effingham, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
All About Cuboid Syndrome
 Cuboid syndrome is a condition where the cuboid bone in the foot becomes partially dislocated, causing pain and discomfort. This small bone, located on the outer side of the foot, plays an important role in maintaining the foot's stability and facilitating movement. Causes of cuboid syndrome often include trauma, such as ankle sprains, or repetitive strain from activities like running and jumping. Poorly fitting shoes and biomechanical abnormalities can also contribute to its development. Symptoms typically involve pain on the outer side of the foot, swelling, and difficulty bearing weight. The pain may worsen with physical activity and improve with rest. Diagnosis is primarily based on physical examination and patient history, as X-rays may not always reveal the issue. Treatment involves realigning the cuboid bone through manipulation by a podiatrist, followed by rest, compression, and elevation. Targeted stretching exercises and orthotic inserts may be recommended to prevent recurrence. If you have persistent foot pain, it is suggested that you consult a podiatrist for further evaluation and treatment.
Cuboid syndrome is a condition where the cuboid bone in the foot becomes partially dislocated, causing pain and discomfort. This small bone, located on the outer side of the foot, plays an important role in maintaining the foot's stability and facilitating movement. Causes of cuboid syndrome often include trauma, such as ankle sprains, or repetitive strain from activities like running and jumping. Poorly fitting shoes and biomechanical abnormalities can also contribute to its development. Symptoms typically involve pain on the outer side of the foot, swelling, and difficulty bearing weight. The pain may worsen with physical activity and improve with rest. Diagnosis is primarily based on physical examination and patient history, as X-rays may not always reveal the issue. Treatment involves realigning the cuboid bone through manipulation by a podiatrist, followed by rest, compression, and elevation. Targeted stretching exercises and orthotic inserts may be recommended to prevent recurrence. If you have persistent foot pain, it is suggested that you consult a podiatrist for further evaluation and treatment.
Cuboid syndrome, also known as cuboid subluxation, occurs when the joints and ligaments near the cuboid bone in the foot become torn. If you have cuboid syndrome, consult with John Killough, DPM from Regional Foot Center. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Cuboid syndrome is a common cause of lateral foot pain, which is pain on the outside of the foot. The condition may happen suddenly due to an ankle sprain, or it may develop slowly overtime from repetitive tension through the bone and surrounding structures.
Causes
The most common causes of cuboid syndrome include:
- Injury – The most common cause of this ailment is an ankle sprain.
- Repetitive Strain – Tension placed through the peroneus longus muscle from repetitive activities such as jumping and running may cause excessive traction on the bone causing it to sublux.
- Altered Foot Biomechanics – Most people suffering from cuboid subluxation have flat feet.
Symptoms
A common symptom of cuboid syndrome is pain along the outside of the foot which can be felt in the ankle and toes. This pain may create walking difficulties and may cause those with the condition to walk with a limp.
Diagnosis
Diagnosis of cuboid syndrome is often difficult, and it is often misdiagnosed. X-rays, MRIs and CT scans often fail to properly show the cuboid subluxation. Although there isn’t a specific test used to diagnose cuboid syndrome, your podiatrist will usually check if pain is felt while pressing firmly on the cuboid bone of your foot.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are ice therapy, rest, exercise, taping, and orthotics.
If you have any questions, please feel free to contact our offices located in Charleston and Effingham, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
All About Cuboid Syndrome
Though cuboid syndrome predominately affects athletes, non-athletes can suffer from it too. Cuboid syndrome is also called cuboid subluxation or cuboid fault syndrome, and occurs when a joint or ligament near the cuboid bone of the foot becomes damaged, or when the bone itself is dislodged from its natural position. Pain may be persistent, or come and go, and it is usually marked by the outside of the foot. Cuboid syndrome, unless severe, can be difficult to diagnose. A doctor will likely ask questions about how long the pain has been present, and will apply pressure on the cuboid bone to determine the origin of pain.
There are a number of causes that can lead to the syndrome. Due to athletic activities, repeated stress placed on the foot can cause cuboid subluxation. Ballet dancers, runners, and other athletes often develop this condition. Basketball or tennis players may also develop this condition, as they place stress on their feet while moving side to side. Cuboid syndrome can often develop over time; however it can come out of a sudden injury as well. Over pronation, or other problems with feet, can exacerbate the condition if not corrected.
Among podiatrists, there is some disagreement about the treatment, as well as the definition of cuboid syndrome. Some see the injury as an injury to the ligaments located nearby the cuboid bone, while others believe it refers to the dislocation of the calcaneal-cuboid joint only. Treatment opinions differ as well. Although it can be treated by manipulation in order to reposition the bone, this must be done with extreme care in order to avoid injury. Some doctors, however, prefer treatment through the use of orthotic pads, designed to keep the bone in its place. Effectiveness of these treatments may vary, according to the severity of the injury.
When you experience side foot pain, it is important that you seek medical assistance. If a subluxed cuboid is caught and treated early, treatment is usually successful, and individuals may begin activities such as sports when the pain subsides. If left untreated, the pain will worsen, and the condition could cause permanent damage.
Arthritis Can Cause Pain in the Feet and Ankles
Symptoms and Risk Factors for Toenail Fungus

Toenail fungus, also known as onychomycosis, is a fungal infection affecting the toenails. It typically begins as a white or yellow spot under the tip of the nail and can spread deeper into the nail over time, causing discoloration, thickening, and crumbling of the nail edges. Risk factors for toenail fungus include frequent exposure to warm and moist environments such as public showers, wearing tight-fitting shoes, and having a weakened immune system. Symptoms may include a foul odor from the infected nail, pain or discomfort, and difficulty trimming the nail due to its thickness. If left untreated, toenail fungus can lead to permanent damage to the nail bed and spread to other nails or skin. The chances of recovery increase when treated early. If you have toenail fungus, it is suggested that you contact a podiatrist where you can receive expert treatment for this condition.
For more information about treatment, contact John Killough, DPM of Regional Foot Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact our offices located in Charleston and Effingham, IL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Toenail Fungus
Toenail fungus is a frustrating problem that affects many people. It can be persistent and hard to get rid of. As many different types of fungi are present throughout the environment, it is very easy to contract toenail fungus.
The feet are especially susceptible to toenail fungus because shoes and socks create the ideal dark and moist environment that fungal infections thrive in. While fungal infections of the nail plate are quite common, if left untreated they can spread beyond the toenail and into the skin and other parts of the body.
Signs of toenail fungus include a thickened nail that has become yellow or brown in color, a foul smell, and debris beneath the nail. The toe may become painful due to the pressure of a thicker nail or the buildup of debris.
Treatment for toenail fungus is most effective during the early stages of an infection. If there is an accumulation of debris beneath the nail plate, an ingrown nail or a more serious infection can occur. While each treatment varies between patients, your podiatrist may prescribe you oral medications, topical liquids and creams, or laser therapy. To determine the best treatment process for you, be sure to visit your podiatrist at the first signs of toenail fungus.
How to Identify and Treat a Foot Corn

Corns, those pesky patches of thickened skin, can turn a simple walk into agony. Identifying them is key. Look for hardened areas on toes or feet, often with a cone-like shape pointing inward. They are caused by friction and pressure, typically from wearing ill-fitting shoes or repetitive actions. Treating corns involves gentle methods like soaking the feet in warm water, using a pumice stone to smooth the area, and moisturizing to prevent recurrence. Avoid over-the-counter corn removal products, as they can damage healthy skin. For persistent corns, or if you are unsure about treatment, it is wise to seek advice from a podiatrist. They can provide professional care, assess your foot health, and recommend appropriate courses of action. Do not let corns slow you down. It is suggested that you schedule an appointment with a podiatrist for personalized guidance and relief.
If you have any concerns regarding your feet and ankles, contact John Killough, DPM of Regional Foot Center. Our doctor will treat your foot and ankle needs.
Corns: What Are They? and How Do You Get Rid of Them?
Corns can be described as areas of the skin that have thickened to the point of becoming painful or irritating. They are often layers and layers of the skin that have become dry and rough, and are normally smaller than calluses.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as wearing:
- Well-fitting socks
- Comfortable shoes that are not tight around your foot
- Shoes that offer support
Treating Corns
Treatment of corns involves removing the dead skin that has built up in the specific area of the foot. Consult with Our doctor to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our offices located in Charleston and Effingham, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Everything You Need to Know About Corns
Corns are hard and thick areas of skin that form as a result of constant rubbing, friction, or pressure on the skin. They are patches of dead skin with a small plug toward the center. They may appear on the tops and sides of toes and can make walking painful.
Soft corns are typically thinner with a white color and rubbery texture. Soft corns tend to appear between the toes. Seed corns are another type of corn that appear in clusters and can be tender if they are on a weight-bearing part of the foot. Seed corns usually appear on the bottom of the foot and are likely caused by a blockage in sweat ducts.
While corns and calluses are somewhat similar, calluses are a bit different. Calluses are a patch of dead skin that can occur anywhere on the body. In comparison to corns, calluses are usually a bit larger in size. However, both corns and calluses are caused by increased friction on the skin.
There are some risk factors that may increase your chances of developing corns and calluses. If you have bunions, hammertoe, or a bone spur, you are more likely to develop a corn or callus on your foot.
While Corns and Calluses tend to disappear when the friction to the affected area ceases, the help of a podiatrist may be useful in the removal process. It is important to remove the dead skin around the area and this may be done in a few different ways. Moisturizing creams may be helpful in softening and removing the dead skin around the callus. You should never use razors or other pedicure equipment to remove your corns. Doing this may worsen your corn or callus and cause infection.
In some cases, corns and calluses may be caused by abnormal foot structure or walking motion. In such a case, you should seek a podiatrist’s assistance in order to correct the issue.
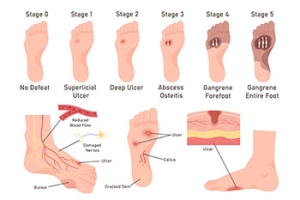
Debridement Methods for Diabetic Foot Ulcers
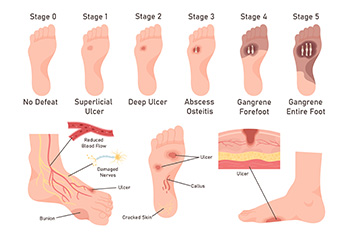
Debridement is a key procedure in managing diabetic foot ulcers, involving a podiatrist removing dead and infected tissue to promote healing and prevent infection spread. This process is vital because the buildup of necrotic tissue can obscure the true extent of the ulcer. There are several methods of debridement. Surgical debridement involves a podiatrist using tools like scalpels to precisely remove dead tissue, often performed at the bedside or in an operating room for more severe cases. Mechanical debridement employs saline-soaked pads that adhere to and remove dead tissue upon removal, though this can be painful and may also disturb healthy tissue. Chemical debridement uses enzymes to dissolve dead material. Biological debridement, utilizing maggots, effectively cleanses wounds by consuming only dead tissue. Before any debridement, the podiatrist will assess the patient’s overall health, and the wound will be cleaned with a saline solution. If you have diabetic foot ulcers, it is suggested that you make a podiatrist a part of your medical team for expert wound care options.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with John Killough, DPM from Regional Foot Center. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our offices located in Charleston and Effingham, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.